Diastasis recti is a separation of the stomach muscles and is fairly common. It can occur at any time, but usually happens in the last trimester and after you have your baby.
What causes it?
During pregnancy, your abdomen gets bigger as your baby grows.
The hormone (relaxin) that causes your muscles to relax for childbirth increases.
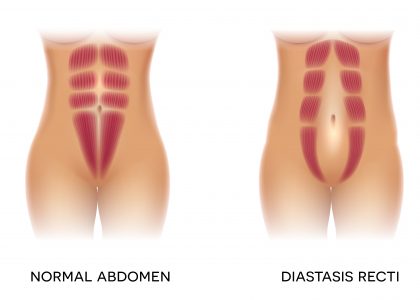
The band of muscle that holds the left and right side of your abdominal muscles together is called the linea alba. Your relaxed muscles and the pressure of your growing uterus causes the linea alba to soften and widen. This is called diastasis recti.
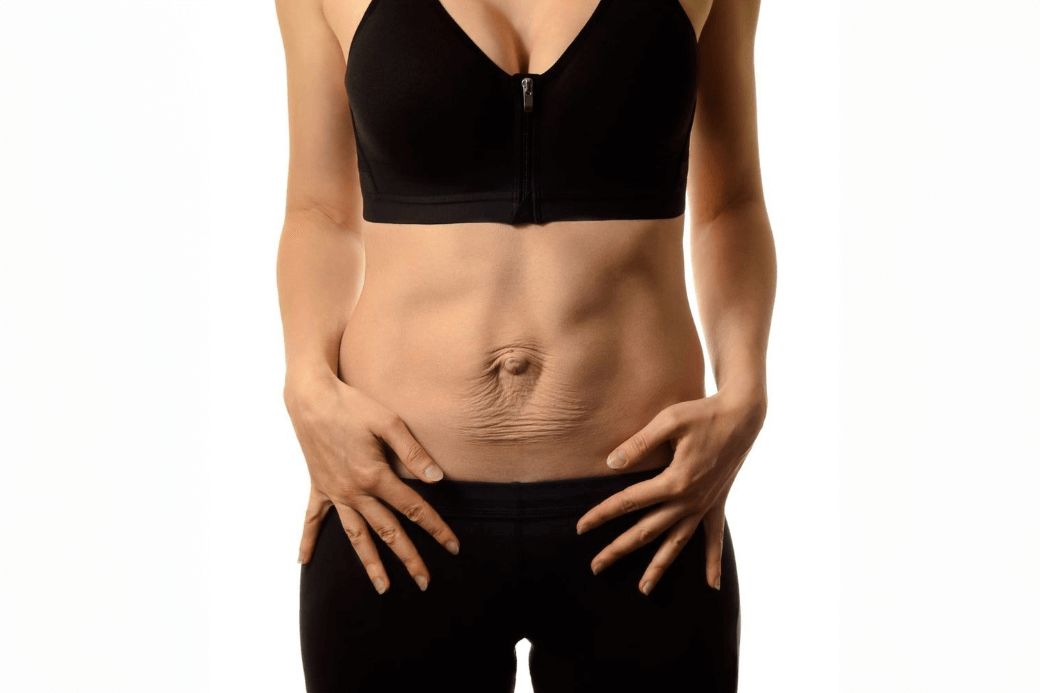
The picture below shows normal abdominal muscles and diastasis recti.
How do I know if I have diastasis recti?
You might notice a separation, ridge or dip in the middle of your abdomen. It can start just under your breastbone and extend to below your belly button. The picture below shows a significant separation.

How to check yourself for diastasis recti:
- Lie on your back with your knees bent and your feet flat on the floor.
- Place your fingertips just below your belly button. Your palm should be facing your head.
- Gently lift your head and shoulders off the floor.
- Feel how far apart your left and right abdominal muscles are.
- Measure the amount of separation using your finger widths. (For example, one, two finger widths)
- A gap of more than two and a half finger widths is considered a big gap.
Why it’s important to treat diastasis recti?
Having diastasis recti means that your abdominal wall is weak. This can affect the strength of your stomach and back muscles which can cause lower back pain. It can also weaken the pelvic floor muscles that support your bladder, rectum and uterus.
With weak pelvic floor muscles you may:
- Leak urine
- Have pain during sex
- Have organ prolapse
If you think you have diastasis recti:
- Talk to your health care provider.
- Talk to a physiotherapist (There are physiotherapists in Manitoba who specialize in pelvic health).
- Your physiotherapist can give you specific exercises to help close your separation
Can I still exercise?
Yes, you can still exercise! However, exercises that push your stomach muscles out can increase the separation and should be avoided. Some examples of exercises to avoid are:
- Abdominal strengthening exercises such as curls, crunches, obliques, sit-ups, “bicycles”
- Abdominal stretching exercises such as yoga poses – “cow pose,” “up-dog,” all backbends and “belly breathing”
- Lifting anything heavier than your baby
References and links
- 2019 Canadian Guideline for physical activity throughout pregnancy
- 2019 Canadian Guideline for physical activity throughout pregnancy (Consensus statement)
- Borg-Stein.J., Fogelman, D., & Ackerman, K. (2011). Exercise, Sports Participation and Musculoskeletal Disorders of Pregnancy and Postpartum. Seminars Neurology, 31(4). 413-422.