Sometimes a parent may make far more milk than their baby needs. Extra pumping, taking herbal supplements or prescription medication (e.g., domperidone) that increase milk supply can lead to oversupply. Parents with too much milk may have frequently engorged breasts/chest which could lead to mastitis or plugged ducts. So how do you know if you have too much milk? And what can you do about it?
You may notice:
- Your breast/chest size growing more than two cup sizes.
- A strong or painful “letdown” of milk once or many times when baby is feeding.
- Milk sprays from the nipple if baby unlatches.
- It is very easy to express your breastmilk/chestmilk.
- The other breast/side of the chest leaks when you are feeding on the opposite breast/side.
- Your breasts/chest feel very full or hard most of the time.
- Frequently blocked ducts or mastitis.
Your baby may:
- Gulp quickly, cough, choke or sputter while feeding at your breast/chest.
- Bite the nipple to try and slow down the milk. They may come off the breast/chest often or not able to stay latched.
- Stiffen their body, arch their back or scream.
- Spit-up and be gassy.
- Have green or watery poop and lots of heavy, wet diapers.
- Gain too much weight quickly.
Did you know?
If you are unsure if you have too much milk, you can check in with your health-care provider or public health nurse.
“I have so much milk and yet my baby still seems hungry”
If you have too much milk, you may be surprised that your baby:
- is hard to settle
- seems unsatisfied
- wants to feed often
This is because your baby is filling up on the foremilk that contains more milk sugar (lactose), which doesn’t keep them feeling full. This also causes a gassy baby and green poops. For more information on foremilk and hindmilk, see Le Leche League’s information on oversupply.
What can help?
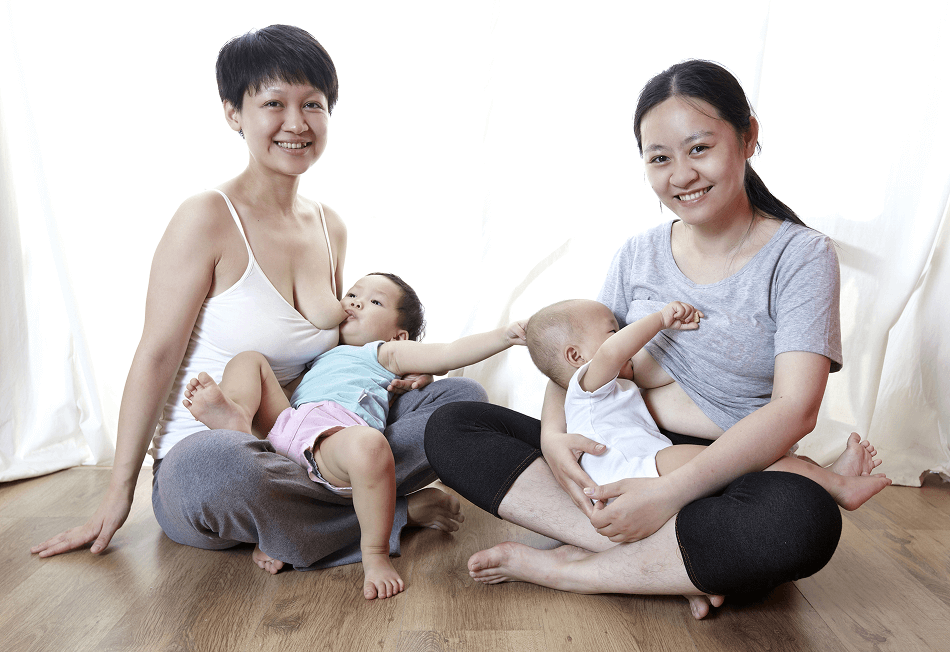
Adjust your breastfeeding/chestfeeding position to one that allows baby’s head to be level with or above the breast/chest. This way:
- Gravity won’t have as much effect on your milk flow.
- Choking is reduced, since milk is directed away from the back of baby’s throat.
Laid-back Nursing
Do the cradle, cross cradle or football hold and then lay back.
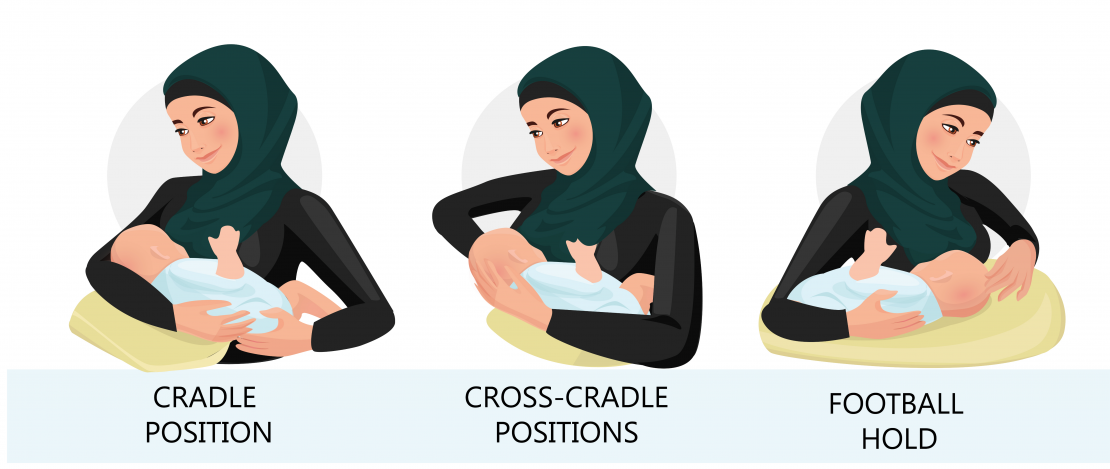

- Get comfortable with your back supported either in bed, on a couch or in a recliner.
- Latch baby using whatever hold you choose (cradle, cross-cradle or football), then lay back so that baby’s head is either at the same level as the breast/chest or above it. You can use pillows to support baby as well.
Side-lying

- Lay down on your side. Use cushions or pillows to support your back, shoulders and neck. Be sure none of these supports are covering or near your baby’s face or head.
- Place baby on their side facing you with their ear, shoulder and hip in a straight line. Pull your baby in close, tummy to tummy. Your baby’s nose should be lined up with your nipple.
- Place a rolled-up towel or baby blanket behind your baby for support. Remember to remove it after you finish feeding.
- Latch baby to your breast/chest.
Baby sitting upright in front

- Find a comfortable position. You may want to support your back and use a footstool for your feet.
- Position baby so they are sitting upright, straddling one of your legs as close to your body as possible. You may need to use a pillow under baby to get them to the level of your nipple. Latch baby to your breast/chest. You may choose to lay back or stay sitting upright.
Safety Tip
When using pillows or rolled up towels or blankets to position yourself or your baby, make sure that none of these supports are covering or near your baby’s face or head. When your baby is finished feeding, place them in a crib, cradle or bassinet for sleep.
How to reduce oversupply if you have too much milk
- Feed your baby based on their hunger cues: Feed your baby as soon as they show signs of hunger (licking their lips, opening and closing the mouth or sucking on their hands/fingers). This is when babies are more likely to suck gently. If you wait until your baby is very hungry, crying and frantic (late hunger cue), they are more likely to suck harder.
- Avoid any extra pumping. If you are separated from your baby or are exclusively pumping, aim to produce only the amount of milk your baby needs and not more.
- Express only a little milk to get relief if your breasts/chest are full.
- Talk to a health-care provider to discontinue any medications or overthe counter supplements that you are taking to increase milk supply.
- Feed with one breast/side of the chest each time. Offer only one breast/side of the chest until baby is satisfied. Switch to the other side on the next feed.
- Block feeding is meant to be a short-term strategy. How to do it:
- Use only one breast/side of the chest to feed baby for a block of three hours. If the other breast/side feels uncomfortable during this block of time, express only enough milk to relieve the pressure.
- After this three-hour time has passed, switch to the other breast/side of the chest for the next three hours.
- Because this reduces your milk supply, you don’t want to continue this for too long. If you have questions or need support, speak with your health-care provider or public health nurse.
If you have a strong letdown:
Express before feeding
Express some milk for one to two minutes before putting baby to your breast/chest. This can help release the first big rush of milk and help slow the flow to an amount that baby can handle.
Un-latch baby when coughing, choking begins
Allow this rush of milk to spray onto a towel or into a sterile container. Re-latch baby once the flow of milk has slowed down. Repeat if it happens again.
Use the scissor-hold on your breast
Use the first and second fingers of your free hand to push the area just above and below the edge of the areola (the darker area around the nipple). Your fingers will look like a pair of scissors. The pressure should slow down the flow of milk. Change the position of your fingers around the areola to avoid blocking the milk duct. You can stop doing this when the flow of milk slows down.